Page 4 of 14
Good clinical practices
Good clinical practice (GCP) is the international ethical, scientific and practical standard to which all clinical research is conducted. Compliance with GCP provides public assurance that the rights, safety and wellbeing of research participants are protected and that research data is reliable. (Definition taken from the National Institute for Health Research)
Ctrl Group consider GCP in their processes, training and the creation of project specific design development plans across all research - not just clinical research. Our compliance with our own practices is monitored in line with our accreditation with ISO 13485:2003 and our approach to each project is outlined in the design development plan for that project.
Your requirements in this regard will vary depending on your product and accreditation, but it is essential that you understand at least the principles.
Background on GCP
Three key factors in the development of Good Clinical Practices were fallout from the Tuskegee experiment, the drawing up of the Nuremberg Code and the Declaration of Helsinki.
The Tuskegee syphilis experiment was an infamous clinical study conducted between 1932 and 1972 by the U.S. Public Health Service to study the natural progression of untreated syphilis in rural African-American men in Alabama.
The 40-year study was controversial for reasons related to ethical standards, primarily because researchers knowingly failed to treat patients appropriately after the 1940s validation of penicillin as an effective cure for the disease they were studying. Revelation in 1972 of study failures by a whistleblower led to major changes in U.S. law and regulation on the protection of participants in clinical studies. Now studies require informed consent, communication of diagnosis, and accurate reporting of test results.
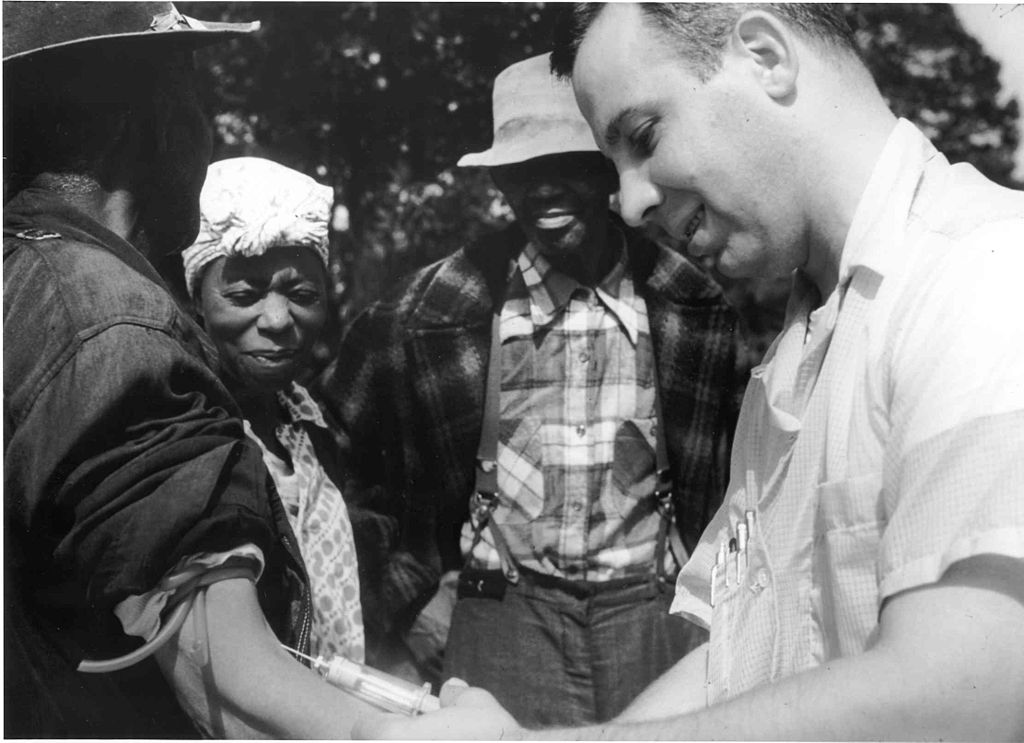 A doctor draws blood from one of the Tuskegee test subjects. National Archives Atlanta, GA (U.S. government)
A doctor draws blood from one of the Tuskegee test subjects. National Archives Atlanta, GA (U.S. government)
The Nuremburg Code
The Nuremburg Code is a set of research ethics principles for human experimentation set as a result of the Subsequent Nuremberg Trials at the end of the Second World War.
The ten points of the Nuremberg Code are:
- Required is the voluntary, well-informed, understanding consent of the human subject in a full legal capacity.
- The experiment should aim at positive results for society that cannot be procured in some other way.
- It should be based on previous knowledge (like, an expectation derived from animal experiments) that justifies the experiment.
- The experiment should be set up in a way that avoids unnecessary physical and mental suffering and injuries.
- It should not be conducted when there is any reason to believe that it implies a risk of death or disabling injury.
- The risks of the experiment should be in proportion to (that is, not exceed) the expected humanitarian benefits.
- Preparations and facilities must be provided that adequately protect the subjects against the experiment’s risks.
- The staff who conduct or take part in the experiment must be fully trained and scientifically qualified.
- The human subjects must be free to immediately quit the experiment at any point when they feel physically or mentally unable to go on.
- Likewise, the medical staff must stop the experiment at any point when they observe that continuation would be dangerous.
The Declaration of Helsinki
The Declaration of Helsinki is a set of ethical principles for human experimentation developed by the World Medical Association (WMA). As Wikipedia says: “It is widely regarded as the cornerstone document on human research ethics”. It covers similar ground to the Nuremberg Code but extends it. We recommend you read the Declaration in full.
GCP principles
The key principles of GCP are:
- Protect the public: Patient/participant/user safety is the utmost importance.
- Help ensure public health: Regulations require that safety information is collected and, depending on the severity, reported to worldwide regulatory authorities so that appropriate action can be taken to protect the public health.
- Provide accurate information: Product labelling provides the consumer and healthcare professional with relevant safety and efficacy information.
- Compliance with regulators: Regulatory authorities mandate drug safety surveillance and adverse effect reporting, and complaint handling including medical device reporting.
Resources
The full GCP guidance from the International Conference on Harmonisation .
GCP impact on design development
GCP can have a huge effect on the work that you do. Within our business, it has an impact on all of the following areas:
- Business Development, Finance & Administration: Recruiting and training people with GCP competence, making sure contracts and agreements, client and business requirements don’t breach GCP principles.
- Study Design & Study Management: Recruiting and training people to manage information in line with GCP. Planning studies that randomise subjects and include appropriate monitoring, statistics and reporting.
- Regulatory Affairs: Ensuring that essential documents including ethics submission, pharmacovigilance and safety reporting are completed and that regulatory affairs are considered.
- Quality Management: Clarity on the recruitment and training of quality management across the project and regular review and updating of the quality management system (QMS).
- Design & Development: Understanding of the requirement for medical device certification, clarity around design development planning and the details of any technical architecture data management and data transfer associated with the product.
Regulatory overview and inspection
In the UK the MHRA GCP inspectorate is responsible for inspecting clinical trials for compliance with good clinical practice. Statutory Instrument (SI) 2004/1031 and its subsequent amendment SI 2006/1928 provide the legal basis for these inspections.
If you’re running a clinical trial, the GCP inspectorate can conduct inspections. It’s to assess compliance with legislation and guidelines on the conduct of clinical trials that involve investigational medicinal products. Each inspector has a legal duty to assess compliance with medicines legislation and holds a royal warrant accordingly.
What is a breach of GCP?
There is considered to be a breach of GCP in a situation where activities are likely to affect the safety, physical or mental integrity of the subjects of the trial or the scientific value of the trial itself.
These breaches are categorised into serious breaches or non-serious breaches.
In the event of a serious breach, the MHRA have stated that they must be notified within 7 days of the sponsor being aware of the serious breach.
Serious breaches would include:
- Mistake in study configuration: Fundamental error in the protocol of the study that compromises the safety of study participants and/or the results that study will produce.
- Scientific mistake: Scientific literature not fully assessed and it is discovered that there are fundamental errors in the scientific background to a scientific reference that is key to the study.
- Project lead or quality manager oversight: A key regulatory or quality milestone has been missed, such as ethical approval.
- Software, hardware or server failure: Software being assessed in the study or used to support the study has fundamental problems or performance issues that compromises the safety of study participants and/or the results that study will produce.
- Theft, damage or loss: Criminal or negligent activity compromises the safety of study participants and/or the results that study will produce.
- Mistake in report: Major conclusions created in a report based on the study findings are not in keeping with the study data.
Non-serious breach might include:
- Mistake in study configuration: A small error in the protocol of the study that does not compromise the safety of study participants and/or the results that study will produce.
- Scientific mistake: Additional scientific discoveries that come to light that you would have referenced in the study protocol if you had known them at the time.
- Project lead or quality manager oversight: A change in project plan or quality management.
- Software, hardware or server failure: Software patch or update is made to remove a bug which is not a major risk to the study participants or the project delivery.
- Theft, damage or loss: Criminal or negligent activity that does not compromise the safety of study participants and/or the results that study will produce.
- Mistake in report: Typos or other small errors in the study reports.
What to do in the event of a breach
We believe in a no blame culture in Ctrl Group. In the event of a breach the study and project leads should be notified immediately, and a process followed to make sure corrective and preventative actions (CAPA) are made.
Notification of a serious study breach is also required by law. Regulation 29A of the full GCP guidance from the Medicines for Human Use (Clinical Trials) Regulations 2004 (Statutory Instrument 2004/1031), as amended by Statutory Instrument 2006/1928 requires notification of “serious breaches” of GCP or the trial protocol.
MHRA have issued guidance on good clinical practice for clinical trials, including reporting serious breaches of GCP.
According to the MHRA, a serious breach needs to be made within 7 days of the sponsor (or whoever this role has been delegated to) being aware of the serious breach.
If the sponsor obtains clear and unequivocal evidence that a serious breach has occurred, the default position should be for the sponsor to notify the MHRA first, within 7 days, and investigate and take action simultaneously or after notification.
In this case, the sponsor should not wait to obtain all of the details of the breach prior to notification. In other cases, some degree of investigation and assessment may be required by the sponsor before notification, to confirm that a serious breach has actually occurred. Apply a pragmatic approach to when you start the clock. Inspectors will review the process for notification during MHRA GCP inspections and delays in notification may be classified as non-compliance. If in doubt about whether and when to notify, contact the quality manager or nominated delegate and if they’re not available, contact the MHRA GCP Inspectorate.
Resources
Government guidance on good clinical practice for clinical trials